Are you tired of persistent nail infections that linger? Bacterial nail infections can be more than just a nuisance – they can impact your daily life and well-being.
In this detailed guide, we will explore everything about managing and treating these annoying diseases. This includes the causes, symptoms, best treatment options as well as preventive measures to avoid it from happening again.
Let’s say bye-bye to discomfort and hi to healthy nails with professional guidance and useful advice. Start here on your journey towards healthier nails!
Understanding Paronychia

Understanding Paronychia Paronychia is a common yet distressing problem affecting the nails which involves an infection in the nail folds, which are important areas of skin around the nails. There are two main types of this condition: acute paronychia and chronic paronychia.
Acute Paronychia
Acute paronychia is typically due to sudden bacterial invasion of Staphylococcus aureus or other pathogens resulting in redness, swelling, pus-filled abscesses surrounding the nail where it grows out of its bed.
Chronic Paronychia
On the contrary, chronic paronychia usually occurs because of repeated exposure to moisture or irritations such as frequent hand washing and biting one’s fingernails thereby weakening their strength.
The proximal nail fold and lateral nail folds are particularly prone to these manifestations while other cases can extend further into deeper locations around the matrix even involving tendons for corrective surgery or removal of nails.
As for those who suffer chronically from these problems, there may be damage at sites like separation between nails themselves along with some kind damage affecting matrices leading to permanent disorders involving their claw-like structure.
Treatment Options
Management options for treating paronychial infections range from topical medications combined with antibiotics against bacterial invaders while steroid creams together with warm soaks relieve pain.
Eliminating factors such as constant washing hands or coming into contact with over-stimulating elements is imperative in preventing relapse when predisposing factors have been identified. Fungicide must be selected to treat onychomycosis, the commonest fungal infection in fingernails and toenails.
Nail Anatomy and Infection

A clear appreciation of how infections like acute paronychia and chronic paronychia take root and affect the nail can only occur when the intricate nail anatomy is understood. The nail consists of a number of important structures including the nail plate, proximal nail fold, lateral nail folds, as well as the bed.
All these play a role in maintaining healthy nails and protecting the nail matrix which is where new cells are made. Acute paronychia usually results from an abrupt bacterial invasion, commonly Staphylococcus aureus or other kinds resulting in inflammation around the nails followed by pus-filled abscesses. This type of infection affects the skin around the fingernails hence it hurts and turns red there.
On the contrary, chronic paronychia occurs slowly due to repeated exposure to moisture or irritations so that skin infection continues for a long time. Some indicators of this condition include onychosis (nail separation) or even changes in appearance such as discoloration caused by fungus that invades both parts – plates and beds.
Such symptoms can get worse with biting or artificial nails or constant wetting. Treatment for fungal infections may differ from those used for other types of bacterial contagions requiring topical antibiotics, systemic antibiotics, surgical treatment along with removals if they persist beyond antifungals.
Types of Paronychia

Paronychia is a grouping term used for describing an infection in either hands or feet that has got two main types: acute paronychia versus chronic paronychia. Each type has different causes, symptoms and treatments available.
Acute Paronychia
Bacterial infection affects the skin encircling the nail, usually the proximal nail fold and lateral folds. This kind of infection is commonly caused by organisms like Staphylococcus aureus, which causes immediate onset of symptoms consisting of redness, swelling and pus filled abscess around the nail plate. This involvement usually has a history of trauma to the nail area like biting nails or presence of artificial nails as well as ingrown nails.
Treatment for acute paronychia usually involves topical antibiotics together with oral antibiotics if it is more severe. Warm water soaks may help reduce inflammation and promote healing while topical steroids can be used to decrease inflammation. When there is no improvement in case of an infection, one may require surgical intervention such as drainage of abscess or removal of nails.
Chronic Paronychia
In chronic paronychia, symptoms occur slowly over time often due to prolonged exposure to wetness or irritants. A combination of factors including regular hand washing, chemical exposure or prolonged fungal infections such as tinea unguium could cause this type of paronychia. The infection targets mainly the nail folds causing chronic inflammation, separation and changes in nail bed.
Unlike acute types where treatment period is relatively shorter that may involve use of topical antifungal agents, warm soaks address underlying causes i.e., too much moisture.
Distinguishing Between Acute and Chronic Paronychia
Differentiating acute from chronic paronychia is important for proper management.
For example, acute paronychia has sudden severe symptoms hence requires early treatment in order to prevent complications.
On the other hand, long term global measures involving combinations with topic treatments including sometimes surgery are required in patients suffering from chronic cases only.
Symptoms and Diagnosis of Paronychia

Successful treatment and management requires understanding its signs as well as diagnosing paronychia. Paronychia falls into two categories, which are acute and chronic paronychia with each having distinct symptoms that require different diagnostic approaches.
Symptoms of Paronychia
Acute Paronychia
- Redness and Swelling: This causes skin inflammation around the nail, usually more noticeable at the proximal nail fold and lateral folds.
- Pus-Filled Abscess: A considerable pus-filled abscess can develop near the nail plate resulting in severe discomfort.
- Pain and Tenderness: Nails usually become very painful when they are infected especially if pressed or touched.
- Fever: In addition to this, there may be other systemic symptoms in some cases such as fever when the condition is severe enough to affect large areas of fingers or toes.
Chronic Paronychia
- Persistent Redness and Swelling: These gradually developing symptoms persist over time unlike the case of acute paronychia which affects nail folds causing continuous irritation.
- Nail Separation: The infection leads to separation of the nail from the bed with consequent discoloration or deformity of it
- Thickened Skin: Continued inflammation makes thickened cracked skin form about nails.
- Fungal Infection Signs: Chronic paronychia exhibits features of fungal infection like discolored or thickened nails often seen in tinea unguium.
Paronychia Diagnosis
An accurate diagnosis of paronychia requires a combination of clinical evaluation and laboratory tests if necessary. This is how paronychia is diagnosed and evaluated:
- Clinical examination: A comprehensive assessment by a family physician or dermatologist is crucial. The healthcare provider will evaluate the infected finger or toenail, looking for signs such as redness, swelling, and pus. The test often involves applying pressure to the affected area to see if an abscess will form.
- Medical History: They would also take into account any predisposing factors such as nail biting, frequent contact with moisture, use of fake nails among others. Any previous history of ingrown toenails or other nail problems will be considered too.
- Lab Tests:
- Swab Cultures: For naming specific bacterial infections or fungal infections, swabs can be cultured from the affected site to identify the causative organism. Common pathogens include Staphylococcus aureus for bacterial infections and various nail fungi for fungal infections.
- Examination Under Microscope: A microscopic examination may be performed on nail samples or skin scrapings in cases where it is suspected that there could be an infection from fungus that causes nails.
- Imaging: In severe or complex cases like X-Rays used to determine complications involving neighboring tendons and bone structures.
- Additional tests: Further diagnostic tests can be conducted if conditions such as squamous cell carcinoma are suspected or if serious systemic diseases are present in patients.
Managing and Treatment of Paronychia
The treatment given after diagnosis depends upon type and severity of paronychia:
- Acute Paronychia: Often it requires oral antibiotics, topical antibiotics and sometimes a surgical procedure for drainage. Warm soaks along with topical steroids help reduce inflammation as well as hasten healing.
- Chronic Paronychia: It encompasses using topical antifungals agents against fungal infections, minimizing exposure to moisture and using topical steroids against inflammation. Long-term management includes avoiding further exposures alongside addressing underlying causes.
Early recognition and understanding of the symptoms of paronychia with prompt medical intervention can help avoid further complications and ensure effective treatment.
Paronychia’s Prevention and Prognosis

When not managed properly, paronychia is a common ailment of the nails that may have serious implications for nail health.
Both acute and chronic paronychia necessitate careful consideration of prevention strategies as well as an understanding of prognosis to ensure effective management and minimize the possibility of recurrence.
Prevention
To address bacterial and fungal infections as well as other issues related to this condition, there are ways through which you can reduce its incidence:
Managing Risk Factors
- Do Not Use Artificial Nails: These types of artificial products hold moisture that readily encourages infections. Use natural means whenever possible.
- Address Ingrown Toenails: This will be a quick treatment given once it is noticed to prevent any future complications. Choose proper medication by consulting medical personnel.
- To take ownership of Pre-Existing Conditions: Underlying conditions, such as diabetes or immunosuppression that can make you prone to nail infections, should be managed by a family physician.
Skin and Nail Protection
- Protect Nail Folds: Avoid trauma on the proximal nail fold and lateral nail folds and use safety measures in high risk activities to prevent injury.
- Use Moisturizers: Apply moisturizing creams to the skin surrounding the nails to avoid dryness and cracking, which are prone to infections.
Prognosis of Paronychia
The prognosis of paronychia depends on the following factors:
Acute Paronychia
- Resolution with Appropriate Treatment: Most cases of acute paronychia respond well if treated with topical antibiotics, oral antibiotics, warm soaks. The severe ones may require surgical treatment as there are pus-filled abscesses.
- Risk of Recurrence: Neglecting predisposing factors like biting nails or exposing them to irritants increases the chances of it reoccurring. Proper hygiene practices applied ensure no future episodes occur.
Chronic Paronychia
- Management with Long-Term Care: For chronic paronychia, long-term treatment may involve topical antifungals and topical steroids. Addressing underlying causes and prevention from further exposure to moisture or irritants is essential for successful management.
- Prognosis for Severe Cases: In severe cases where an extremely damaged or separated nail is present, prognosis may not be good at all. At times resolution might only be achieved through surgery or removal of the nail itself.
Complications and Monitoring
- Monitor for Complications: Monitor any complications like skin infections, disorders of nails or involvement of underlying tendons. Following up regularly by a health caregiver helps in identifying developing issues before they become serious problems.
- Avoid Progression: Untreated or poorly managed paronychia can lead to infection spreading or more severe conditions. Therefore early diagnosis towards better prognosis.
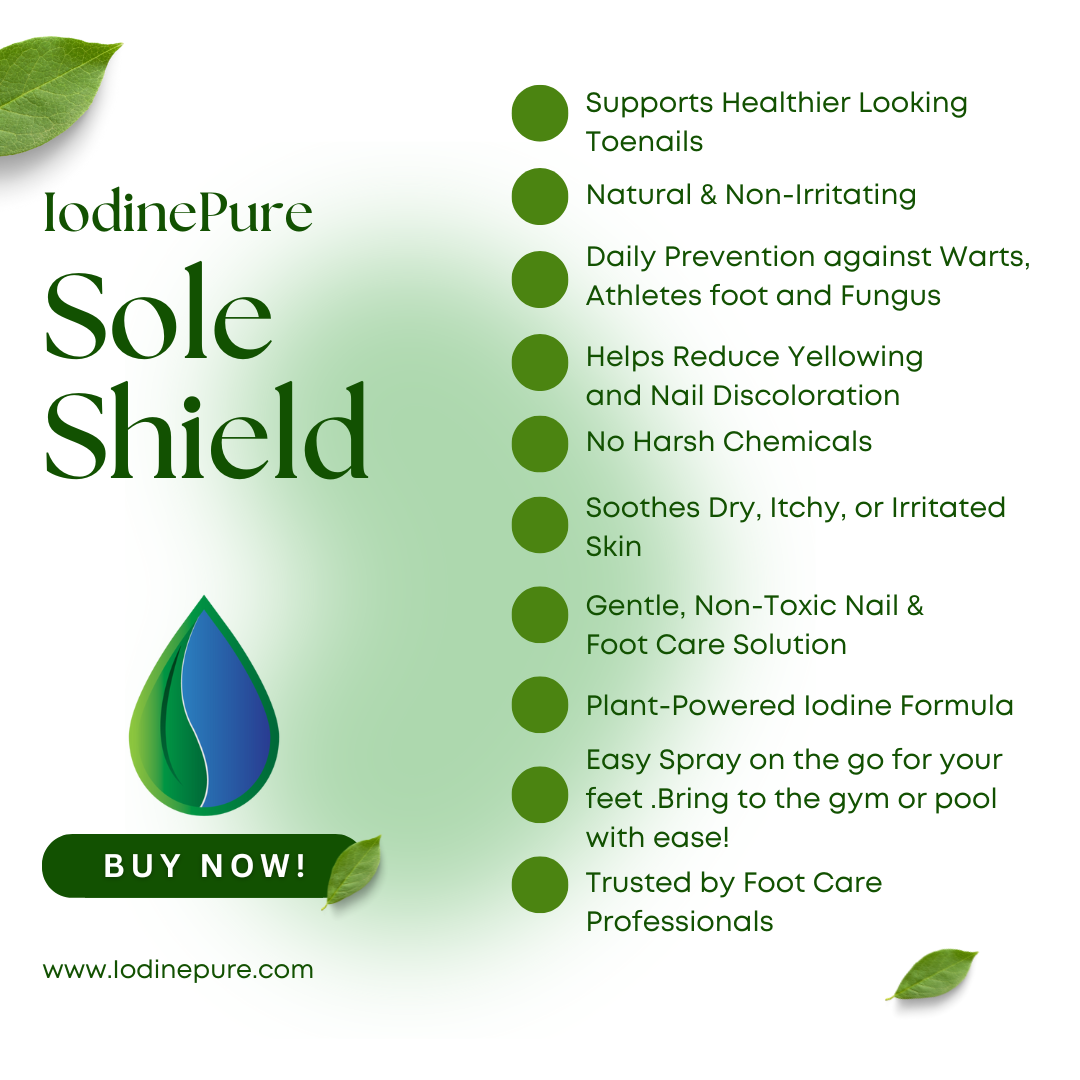
Using EZ Clear Nails to Treat Nail Infections

Easy Clear Nails, is a 100% pure iodine soak that acts as an all-natural fungicide.
EZ Clear Nails is a natural iodine soak designed for nail care, particularly effective as a fungicide. Users should avoid it if sensitive to iodine, allergic to seafood, have thyroid conditions, or ingest it.
Direction for Use
- Place the toes in the toe pan. Pour liquid into the toe pan until the nail is fully submerged.
- For best results, soak for 15 minutes 3 times a week.
- Allow to air dry.
Frequently Asked Questions (FAQs)
Can paronychia be treated at home?
Mild cases of acute paronychia can usually be treated at home with warm soaks and topical antibiotics. Chronic paronychia may require long-term management and monitoring by a healthcare provider.
How long does it take for paronychia to heal?
The healing time for paronychia depends on the type and severity of the infection, as well as proper treatment. Mild cases may heal within a few days, while more severe cases may take several weeks or longer to resolve.
Is paronychia contagious?
Paronychia itself is not contagious, but the bacteria or fungi causing it can be spread to others through contact with infected nails or nail tools. It is important to practice good hygiene and avoid sharing personal nail care items.
Can I prevent paronychia from happening again?
Yes, you can prevent paronychia from recurring by following proper hygiene practices, avoiding irritants and trauma to the nails, addressing underlying conditions, and seeking early treatment for any signs of infection. Regular monitoring and follow-up also help prevent complications and recurrence.